*This is part of UF Explore magazine’s CSI: Alzheimer’s. Click here to read the full story or listen above.
Click here to read Part 3: Superagers.
By Michelle Koidin Jaffee
It’s routine for patients with certain heart conditions to have their cardiac function checked before surgery for a non-heart-related issue, such as a knee operation. But it’s not routine for certain patients who are at risk of cognitive complications to have a presurgery brain check.
UF neuropsychologist Catherine Price wants to change that.
In 2017, Price founded a first-of-its-kind clinic at UF Health Shands Hospital that provides presurgery screening for adults over age 65 to detect any form of cognitive impairment, from mild impairment to more severe forms such as Alzheimer’s disease or other dementias. Four years later, more than 1,000 patients a year go through screening at the clinic, called the Perioperative Cognitive Anesthesia Network.
Although adults over 65 commonly undergo surgery for urgent medical reasons as well as quality-of-life ones like joint replacement, there is a lack of evidence-based, perioperative medical care in older adults with cognitive impairment, Price says.
It’s estimated that 20% of seniors preparing for surgery have preexisting signs of neurocognitive disorders, research by Price and others shows, and such underlying conditions elevate the risk of complications like delirium. Delirium is an acute state of confusion and disrupted attention that is associated with longer hospital stays.
“We need to identify vulnerable people before surgery,” she says. “There needs to be a change in the way clinicians adjust patient care based on brain profiles. People with neurodegenerative disease risk factors and diagnoses require special consideration when it comes to anesthesia and surgery procedure choices.”

The Perioperative Cognitive Anesthesia Network team includes anesthesiologists, neuroscientists, neurologists, surgeons, biomedical engineers and experts in artificial intelligence, and it has clinical, research and training goals. Funded by the National Institutes of Health, it is considered a model nationwide, says UF anesthesiologist Patrick Tighe, co-director of the program.
“Now, if you go to the anesthesiology national meetings, presurgical cognition is a hot topic,” Tighe says. At a pre-pandemic American Society of Anesthesiologists general assembly, he says, Price’s work was held up as “the idealized example so far of how to do presurgical cognitive assessments.”
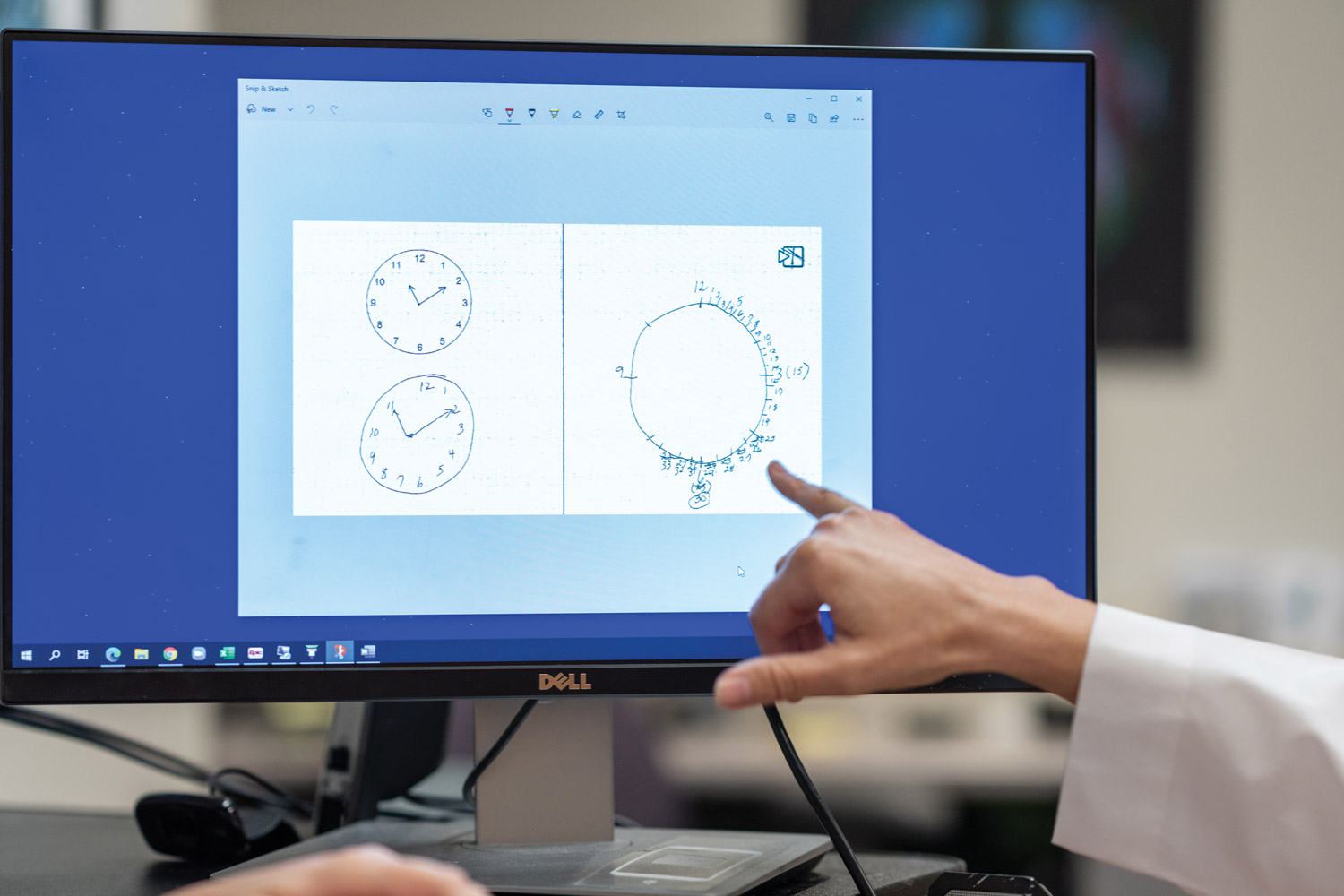
Under the program, cognitive assessment begins with drawing an analog clock using a high-tech pen equipped with a tiny camera that captures images 80 times per second. The image is analyzed by neuropsychologists to determine if further cognitive testing and neuroimaging scans are needed.
The clinic, also led by neuropsychologist Kristin Hamlet, then produces a report to inform anesthesiologists, surgeons, geriatricians and primary care doctors about a patient’s cognitive status and provides personalized recommendations, such as use of a special monitor that assesses the depth of sedation during surgery or adjusting the dosage of certain drugs used for sedation or nausea.
Under ongoing research, the clock drawing is also run through an artificial intelligence algorithm as a tool to make a prediction of cognitive outcomes, Tighe says.
A next important step, says Price, is a large, multisite study using artificial intelligence to analyze medical records to predict outcomes for people with preexisting dementia who undergo surgery.

